R&R#3: How to Prevent and Eliminate the Most Deaths
The aging related failure of the heart and lungs leads to over half of deaths in developed countries. There is reason to be optimistic and much work to be done.
Developing effective treatments for aging diseases is in general one of the most effective ways to eliminate needless death worldwide. But what subset of aging disease causes disproportionate death? What does the evolving standard-of-care look like, and how can the biomedical R&D community optimally target its efforts to make a therapy which causes to largest reduction in preventable death in the least amount of time (and is widely accessible)? This, after all, is the often-stated value of targeting aging damage as a high priority.
Two organs whose failure disproportionately causes death are the heart and lungs. These two organs work closely together to pump oxygenated blood and remove CO2 buildup throughout your body. They are physically very close together, making up the two major organs in your thoracic cavity. It is even possible to transplant them together as a single unit, though there is generally a shortage of viable organs.
The heart and lungs are absolutely essential to survival, given that cells’ most urgent metabolic needs revolve around maintaining a supply of oxygen (neurons for example may die within minutes without an oxygen supply). Additionally, the heart and lungs are in some ways more vulnerable to acute failure than other vital organs such as the kidney and liver. Some characteristics which I consider to facilitate this: The heart is particularly vulnerable in that it is a single, complex structure which is highly metabolically active and prone to damage from atherosclerosis-induced ischemia (a heart attack), and also composed of cells which do not regenerate once lost (cardiomyocytes). With lungs, at least you have two of them, however they are directly exposed to environmental pathogens and toxins.
Regardless of the reason though, it’s undebatable that together their failure cause a substantial proportion of deaths worldwide. Note that together with other cardiovascular diseases (mainly stroke) they cause over half of all deaths in developed countries. Below I’ve plotted a pie graph based on the World Bank High Income statistics between 1990 and 2019 (pulled from ourworldindata.org) demonstrating this. A few caveats to the method:
Lung diseases were not separated out by age, but in each case the vast majority of deaths are known to be age-related
As cancer statistics were lumped together, I divided them into 23% lung cancers and 77% other cancers
As mentioned, strokes are included in cardiovascular disease as the dataset didn’t specify for heart diseases specifically. Thus, the number relating specifically to the heart and lungs is less than 50%
Cancers are usually age-related, but I included them separate to “other aging”
Causes of death: >50% are from cardiovascular disease, lung cancer, COPD or respiratory infection
While heart disease has the reputation of being caused by poor eating habits and lung disease from smoking, aging plays a critical role in the development of all of these diseases regardless of lifestyle, and the risk of their occurrence escalates exponentially with advancing age (see below). However, the pathophysiology of these conditions as it relates to aging is highly multifaceted.
Correlation between age and chronic diseases (see reference on image)·
In the heart, the most popularly known form of damage is atherosclerosis of the coronary arteries which can result in heart attack (and then often results in future cardiomyocyte (heart muscle cell) loss and heart failure due to unrepaired damage in survivors). Atherosclerotic lesion formation is ubiquitous with aging independent of diet. Additionally, direct heart tissue aging is also a major issue though, and is driven by a number of factors spanning the traditional aging hallmarks such as mitochondrial dysfunction and lipofuscin accumulation. Heart failure can also be driven by amyloid accumulation (particularly transthyretin amyloid), which has been termed “senile systemic amyloidosis” and is a disproportionate killer of the extremely old.
Similarly, in the case of pulmonary diseases like COPD and lung cancer, aging is a significant risk factor. Aging lungs lose their elasticity and endure multiple forms of damage both at the cellular level and within the extracellular matrix, including fibrosis. Lungs are very large, actively mitotic organs as well, and coupled with high levels of environmental DNA damage present, this means that lung cancer is by far the most common cause of cancer death in developed countries. Both COPD and lung cancer have been tied to the nine hallmarks of aging to varying degrees. Lastly, pneumonia is a major killer primarily in the very old due to a combination of the above-mentioned lung aging damage as well as immune system aging.
The fine details of aging in these two tissues deserves an article unto its own, but the overarching point is that the aging of these two tissues is among the greatest killer of human beings.
The standard-of-care for managing heart failure involves a complex regimen of multiple medications, a practice often referred to as polypharmacy. Standard treatment guidelines start patients on up to 4 medications, and during worsening heart failure or acute decompensation events more may be added. The end result of all of this is more medications than can be counted on one hand and death pushed back only a few years (as none of these medications reverses damage). The average cost per heart failure patient is estimated at $24,383 (including medications as well as heart-failure specific hospitalizations.
For COPD, the treatment often includes long-acting bronchodilators to help keep the airways open and inhaled corticosteroids to reduce inflammation. In instances of acute exacerbations, it also becomes necessary to use additional therapies like antibiotics, systemic corticosteroids, and supplemental oxygen. However, despite these interventions, the disease is also typically progressive, leading to a decline in patient health over time. While the goals in the case of lung cancer and pneumonia are curative, the underlying aging damage will notably still not be reversed even if therapy is successful.
Part 3: Strategies for Whole Heart and Lung Replacements
Given the high disease burden and the limitations of current therapies, there is an increased focus on solutions which target the underlying problems (the aging damage in the tissues) and can either cause rejuvenation or replace the organ entirely.
Aging therapeutics functioning at a cellular level have promise in these diseases. There is a significant amount of exciting work being done to combat atherosclerosis by removing plaque (1,2,3), which could significantly reduce heart attack frequency. Mitochondrial therapeutics could have major benefits for heart failure, as well as senolytics in both heart disease and lung disease
Cell therapy is also an active interest in heart failure treatment research. Current evidence suggests that most treatments fail to actually regenerate cardiomyocytes and work via indirect means, however there are some promising exceptions. Mesenchymal Stem Cells (MSCs) treated with mRNA to mimic genes involved in cardiac development have been used to generate stem cells capable of differentiating to a cardiomyocyte-like state, and were able to improve cardiac performance post heart-attack. The first human trial of induced Pluripotent Stem Cell (stem cells derived from adult cells) derived cardiomyocytes to treat heart failure was recently initiated.
A number of clinical trials have tested stem cells, primarily adipose or bone marrow derived MSCs, in COPD, with primarily positive safety and some degree of success. The actual function through which the treatment is acting appears to again be ambiguous though, with symptom-based outcomes generally measured rather than rejuvenation. SMS biotech is utilizing adult Small Mobile Stem cells along with engineered extracellular matrix to induce rejuvenation, with COPD as a leading indication in “FDA” phase according to the company pipeline (presumably near Investigational New Drug (IND) and Phase 1 initiation)
The field of tissue engineering holds great promise given a fairly straightforward point to work back from (a functioning. As mentioned previously, heart transplants and lung transplants are performed regularly and can be performed together, and the primary limitations at the moment are regarding a dearth of viable donors. One company, eGenesis, is using CRISPR gene-editing technology to create pig organs that are compatible with human recipients, lists heart as a major organ of interest in its pipeline. I’m unaware of any tissue engineering focused companies working on growing lungs, though academic work is going on in the area, and a 2018 paper showed that bioengineered lungs could be successfully grown on decellularized scaffolds and transplanted into pigs.
Theoretically, they are exceptionally hard tissues to grow in a laboratory for several reasons. Lungs are extremely densely vascularized and have a very complex internal structure composed of branching alveoli, and the work mentioned above is using decellularized lung scaffolds as a starting point. Heart development is exceptionally complex in that it involves the complex looping and folding of tubes to create a final structure which must be precisely mechanically tuned.
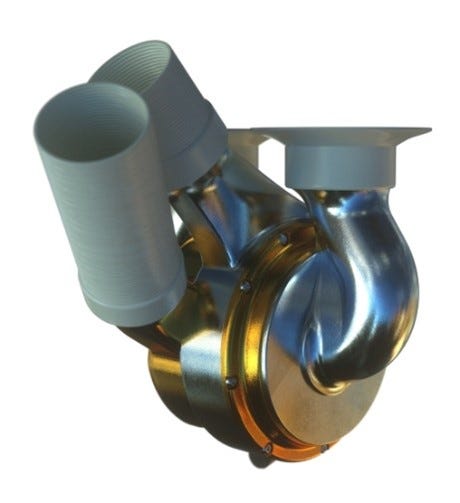
More mature in the development pipeline for these two organs are artificial organ technologies. Though it may seem to some to be something out of science fiction, the heart and lungs in my opinion represent examples where artificial replacement could be a great option. They do not contribute directly to consciousness as the nervous system does, nor to outwardly observed identity. Moreover, they are organs whose primary functions are mechanical (in the case of the heart) or for straightforward gas exchange (in the case of the lungs), lacking an end goal of complex metabolism as in organs such as the liver. Artificial hearts, in fact, have been available as a temporary solution for patients awaiting transplant for some time, with well known examples include the SynCardia temporary Total Artificial Heart (TAH) and the Carmat TAH. BiVACOR TAH, a newer device, employs a simpler, more durable design that eliminates wear-prone parts, potentially capable of permanently replacing the human heart. Utilizing a full metal design incorporating a magnetically rotated centrifugal impeller, it may also avoid some issues observed in the other heart. The first in human studies are likely to begin in the next few years, with the company recently having raised an additional round of funding.
Extracorporeal Membrane Oxygenation (ECMO) using a heart-lung machine utilize a large external machine in a hospital setting to take over the function of both organs, often during surgery. The more novel lung "backpacks" are a portable form of ECMO shown to work in sheep and nearing clinical testing, which could provide the opportunity for extended use without being immobilized. Still too big to be implanted, they nonetheless would be a significant step.
(Top) Bivacor heart, (Bottom) Wearable artificial lung from University of Pittsburgh
Development of an implantable artificial lung notably faces challenges associated with the tradeoff between the need for high internal surface area (and thus densely packed capillaries for gaseous diffusion) and the need to avoid clot formation. Microfluidics (basically, really small channels for liquid to flow) offers a possible solution for the first point, and varying techniques including adding endothelial cells or heparin to prevent clotting have been tried. The development of implantable artificial hearts is in comparison more advanced. It is also worth noting, as alluded to previously, that combined transplants are a theoretical option if both tissues have a heavy load of aging damage and active or imminent disease. I imagine that this could reduce the need for multiple operations and even enable crosstalk between the new heart and lungs which may have multiple benefits.
What is the best treatment to focus resources and focus on in each case? Whole organ solutions offer long-term solutions, with tradeoffs between biological options versus artificial, though are somewhat further off (lung more-so than heart). Repairing aging damage such as eliminating senescent cells or restoring mitochondrial function offers a tractable shorter-term solution, and cell therapy lies somewhere in between. However, all are in theory superior both effect-wise and cost-wise versus the current compensatory multi-drug strategy, as they would not require long-term administration and could have a more lasting ability to reduce hospitalization rates. I personally believe that all these options should be pursued in parallel as they are now, but exceptionally aggressively given the tissues’ disproportionate effect on lifespan. In an ideal scenario where all strategies were developed, aging damage repair and cell therapies could be given periodically until/unless some insurmountable factor required whole organ replacement.
(Above) My thoughts on repair and rejuvenation techniques in the heart and lungs
One additional question, however, is as to what the biggest roadblock to developing these therapies is. In my opinion, interest (and thus funding as well) is limited primarily given the lack of previous successes. All major players in the healthcare system lack a concrete paradigm of what a future where we have these types of tools will look like, including doctors and caregivers, insurers, drug companies, patients, and regulators. Thus many people are still thinking principally in terms of what the next drug in the standard treatment cocktail will be. However, the first transformative rejuvenation therapy will open the doors for many others.
Imagine that an artificial heart which results in a 95% reduction in cardiac disease mortality, and eliminates the need for polypharmacy and frequent hospitalization, comes out tomorrow. Almost everyone knows someone with heart disease – you won’t need to be an expert or to look at the news or to blog articles on the subject to appreciate the significance and the implications for society’s (and your own) future. And in a perfect scenario where mortality related to cardiovascular disease and lung disease was entirely eliminated, including all atherosclerosis (which I hope to go into depth in in another article) and thus stroke as well, a little over half of all deaths would be prevented. It’s a somewhat wide bucket and a tall order still, but I believe it’s far from impossible to see within a generation.