R&R#1: SCD, A Treatment Paradigm Evolving Towards Durable Rejuvenation Treatments
What is an optimum therapy? Can this be generalized across diseases/indications?
One of my favorite parts of the aging and lifespan/healthspan community is that it implicitly has an ideal benchmark for success. That is, in an ideal scenario a diseases tissue would be brought indefinitely to a non-diseased biological state, characterized not only by symptom relief but also ideally by physiological youthfulness at the tissue, cellular, organelle, and genomic/epigenomic/transcriptomic/proteomic levels. In principle, once physiology is restored in this way we don’t need further treatments until many additional years of entropy take their toll.
Is this easy? Clearly not, as aging is multifactorial and aging diseases like NASH and Alzheimer’s are notoriously hard to treat. In the absence of such options, treatments have mostly targeted signalling pathways and have been symptom-reducing, or moderately damage-slowing at best. Success is thus more defined on a shorter term, requiring sufficient symptomatic improvement over the Standard-of-Care (SoC) to validate inclusion in the clinical treatment paradigm and justify pricing and high market share.
My underlying guiding principle is that medicine should reduce human suffering and enable people to thrive. Thus, all improvements to the treatment paradigms of diseases affecting tens of millions of people are transformative. But, with the current paradigm we sadly face a lack of sustainability driven by the fact that optimum health is essentially an infinite limit which cannot be reached with increasing numbers of compensatory treatments. This is one of the main reasons healthcare systems are hemorrhaging across the world, and perhaps the central message I want to focus on in this blog is that this will only improve by repairing underlying damage and rejuvenating tissue.
So, what does that course look like? Today I’d like to look at a devastating and exemplary indication… which has nothing to do with aging! But for real, Sickle Cell Disease is a disease whose treatment has evolved over the past several decades in a way from which many parallels can be drawn regarding large-scale impact.
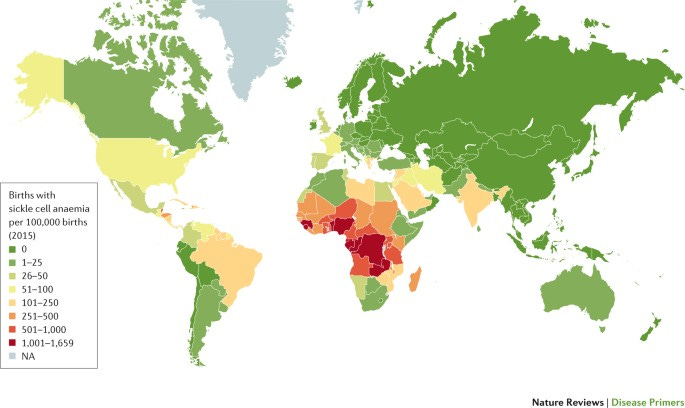
Sickle Cell Disease (SCD) is among the most common rare diseases that exists, with an estimated 100,000 patients in the US and millions in Africa. It is a monogenic, autosomal recessive disease resulting from a mutation in the HBB (hemoglobin gene). Red blood cells (RBCs) attain a classic sickled shape as a result, which can cause a number of severe health issues including anemia and Vaso-Occlusive Crisis (VOCs) (more on these later). Interestingly, heterozygous individuals (called Sickle Cell Trait) have significantly increased resistance to malaria, thought to be why this allele has persisted at relatively high levels in populations historically from malaria prone regions such as sub-saharan Africa. For this reason the disease largely is found in disadvantaged ethnic groups, and patients may be exceptionally cost-sensitive (especially where healthcare systems are weak) and struggle to get needed treatments.
SCD Frequency, Kato et al 2018
Complications of the disease define the standard primary and secondary endpoints off of which SCD therapies are assessed in trials and in the clinical treatment paradigm. One is anemia, caused by the reduced capacity of the RBCs to carry oxygen, and generally assessed therapeutically by total increase in hemoglobin per volume of blood. The other most notable type are VOCs, where the sickled cells occlude blood vessels due to their unusual shape and cause severe pain and potentially more severe complications. VOCs are generally assessed by prophylactic reduction in frequency, and existing treatments don’t acutely stop VOCs. Additional considerations are various forms of long-term organ damage in the kidney, lungs, heart, brain, liver and elsewhere. Therapeutics may target some or all of these endpoints, and SCD patients have significantly reduced lifespan on average.
So, to the point, modern SCD treatment began by incorporation of straightforward but expensive treatments such as blood transfusions, which remain a mainstay today. Eventually doctors began to incorporate a simple small-molecule called hydroxyurea as a first-line pharmaceutical therapy, first approved by the FDA for the indication in 1998. Hydroxyurea increases expression of another, special hemoglobin gene usually only activated in fetal development (called HBF) and thus targets a relevant signalling pathway to reduce damage due to the disease. A branded formulation of hydroxyurea, Siklos, reduced VOCs and hospitalization rates by a little under half over a 1-year period. Hydroxyurea is also cheap, at a little over $50 for 100 capsules. However, SCD remains so expensive in the US at over $1.5M over a lifetime that cost offset alone very easily justifies further treatments, potentially much more expensive ones.
The next-line of treatments generated to fill that gap further improved symptoms, but were novel molecules on-patent and thus much more expensive. Voxeletor (Oxbryta) is an oxygen affinity modulator developed by Global Blood Therapeutics (recently bought by Pfizer for $5.4B) which was approved in late 2019 and increased hemoglobin by >1g/dL in 51% of patients vs 7% for placebo (~2/3 of placebo were on hydroxyurea). This is a meaningful but non-curative improvement which was criticized by ICER (the Insitute for Clinical and Economic Review) for its high price of over $10k per month at the time. Even more notably, the other drug criticized for high prices on the review, crizanlizumab (Adakveo), which reduces P-selectin and thus reduces RBC occlusion of blood vessels and consequently VOCs, was also approved in 2019 after a Phase 2 trial success just to fail a subsequent larger Phase 3 trial this year. It now sadly faces potential removal from the shelves not long after it reached them in the first place.
Several other treatments were being tested which modulate other pathways to increase HBF or HBB. Imara’s tovinotrine failed to show significant improvement in 2022. Agios’ mitapivat (PKR activator) is being tested in a Phase 2/3 study, and if approved would likely also be fairly high-priced using its >$300k annual price in Pyruvate Kinase Deficiency as a benchmark (albeit PKD has a much smaller patient population so it would certainly be less than this in SCD). Forma Therapeutics' etavopivat is also a pyruvate kinase activator in a Phase 2/3 trial. Several other compounds are in earlier phase trials as well.
At ~$100k/year (estimate based approximatelyon the cost of voxeletor), a patient on one of these compounds for 40 years of their lifespan would spend $4M on the drug. This effectively excludes the possible use of multiple expensive, new-generation therapies from a cost perspective. But, what if we could have a one-off, more effective treatment which restores us at or close to the healthy tissue benchmark (in this case, that of non-SCD patients)? Enter gene therapies.
Overview of SCD Therapy Development, Salinas Cisneros and Thein 2020
In the case of SCD, curative approaches utilizing Hematopoetic Stem Cell (HSC) transplants from healthy patients have existed for a few decades. Unfortunately, these are both limited by the number of donors and come with the immunogenic risks inherent in allogenic transplants such as Graft-Versus-Host Disease (GVHD), as well as major risks generally inherent with the transplant itself. More recently, the first two of these three issues have been addressed by gene therapies applied to a patients own HSCs in culture (ex vivo) and added back in. In fact, as a severe disease justifying a fairly high price tag and yet still having a large population, SCD has attracted multiple gene therapy players. First to the stage was Bluebird Bio, who are developing a therapy called lovo-cel, a gene insert expressing a shRNA which inhibits BCL11A (itself an inhibitor of HBF) to the RBCs. This was recently submitted for a BLA and promises to be a major landmark for gene therapy if approved. The therapy was arguably curative, reducing VOC rates to zero in most cases and majorly increasing hemoglobin levels. CRISPR therapeutics Exa-Cel was also just submitted for a BLA, silencing BCL11A directly via a CRISPR-based strategy and similarly showing outstanding results. Despite the continuing risk of HSC transpant associated with these treatments prospective patients have overall shown significant positivity regarding the prospect.
What does this mean from a cost-perspective? In principle, the huge cost of SCD even with modern treatments noted above leaves huge room for pricing based on a cost-offset model, whereas the end price is justified by the amount it saves insurers in other costs (including other drugs, transfusions, acute VOC hospitalization and treatment, etc). ICER recently stated that it would consider a price as high as $1.93 million to be cost-effective. Another study suggested that a cost of $2.18M would be cost-effective to the US healthcare system, explaining their logic in detail. While people often do a double-take when first introduced to the price of a gene therapy, this is notably less than the price of expensive drugs which need to be taken indefinitely such as those listed previously.
Cost-Effective Durable Therapies for SCD Justify Higher Values than SoC. Salcedo et al 2021
A further reason for optimism, though, is that several factors are likely to drive these prices down majorly over time. The first to take effect and most obvious is competition- two great therapies are likely coming into the field at almost exactly the same time and could potentially justify first-choice on a formulary through reduced cost vs the other. Second is eventual loss of exclusivity, though it’s unclear what barriers will exist to generic entry of gene therapies. And third is the potential for in vivo treatment eventually (no HSC transplant required) or improvements in HSC transplants which would reduce the underlying cost (and risk). Imagine a world 1-2 decades in the future where multiple gene therapy biosimilars are available for under $50,000 including the cost of the treatment itself, and a patient spends a few days in the hospital at max. It’s ambitious but far from impossible, and with the correct local discounts and rebates it could even be a strategy applied in African countries where supply chains and patient distance from treatment centers can make recurring therapy difficult.
SO, what is the implication of all of this for aging medicine? I would compare most to either hydroxyurea or the second-generation therapies as of now. Some treatments are cheap and widely prescribed to older individuals with beneficial effects reducing long-term risk but eventually failing to overcome the progression of tissue damage. For example, statins for cholesterol, beta-blockers and ACE inhibitors for heart failure, and metformin for type-2 diabetes, etc. Other, newer therapies improve notably on these drugs but are expensive and are only prescribed when diseases are worsening, such as PCSK9 inhibitors for cholesterol, sacubitril/valsartan (Entresto) for heart failure, and SGLT inhibitors for diabetes. They are meaningful improvements helping many people live better lives, but what is the next step?
Unlike SCD which is a monogenic disease, restoring initial physiology in aging indications is less straightforward. A few gene therapies are being developed, such as APOE-targeted Alzheimer’s therapies by Lexeo therapeutics or the multi-gene therapy approach pursued by Rejuvenate Bio. But in general, multi-modal approaches are needed, and those being developed by the aging field can get us there. For atherosclerosis for example, people will develop it eventually regardless of the above cholesterol medications (or however much they exercise and how many cheeseburgers they eat), but multiple companies such as Cyclarity, Elastrin and Repair Bio are now working on removing different modalities of underlying damage. And in the case of chronic aging diseases, while the initial cost offset is certainly not $2M per patient, the patient population sizes are enormous and the costs make up the majority of annual healthcare expidentures. Thus, while the pathway may be harder than in SCD and other genetic diseases, the end payout of reaching out directly to the finish line and shooting for the optimum therapy in aging diseases is far, far too great to be ignored, both in terms of costs-saved and human lives saved. This is the way, the north star that we must work towards. As one of my favorite quotes goes:
“Set a course. Take it slow. Make it happen…” -Battlecruiser captain, starcraft