R&R#2: Treating Aging Diseases is the Obvious Answer to Demographic Aging
Though it will take some visible success stories initially, the world is poised to realize this.
Articles on demographic aging as a looming economic crisis are quite common in the news today. I was drawn to write about this topic after reading an article in The Economist, but it is one among many with relatively similar points: societies, economies, and particularly healthcare systems become more at risk of collapse as a higher % of the total population reaches a biological age where productivity and independence are inhibited.
The concept itself can’t really be debated, so I won’t go into too much depth discussing it. Basically, two factors have changed significantly in the world leading to the current situation. One is falling fertility rates, initially occurring primarily in east Asia and eastern Europe but now below replacement rates in most countries other than those in sub-saharan Africa, central Asia and more underdeveloped regions of the middle east. Efforts to reduce demographic aging often have focused on increasing fertility rates, from China’s recent elimination of the one-child policy to efforts elsewhere to subsidize childcare and/or give direct subsidies and thus improve the cost-benefit ratio for those considering on having kids. However, clear long-term trend reversals are lacking, and birthrates in China have continued to drop. Limited global birth rate decline is not necessarily by itself a bad thing, likely leads to as well as derives from enhanced freedom and opportunities for women, and efforts to increase birth rates locally are at times driven in-part by nationalist sentiment and have in their extremes even been crushingly bad for women’s freedoms in the past.
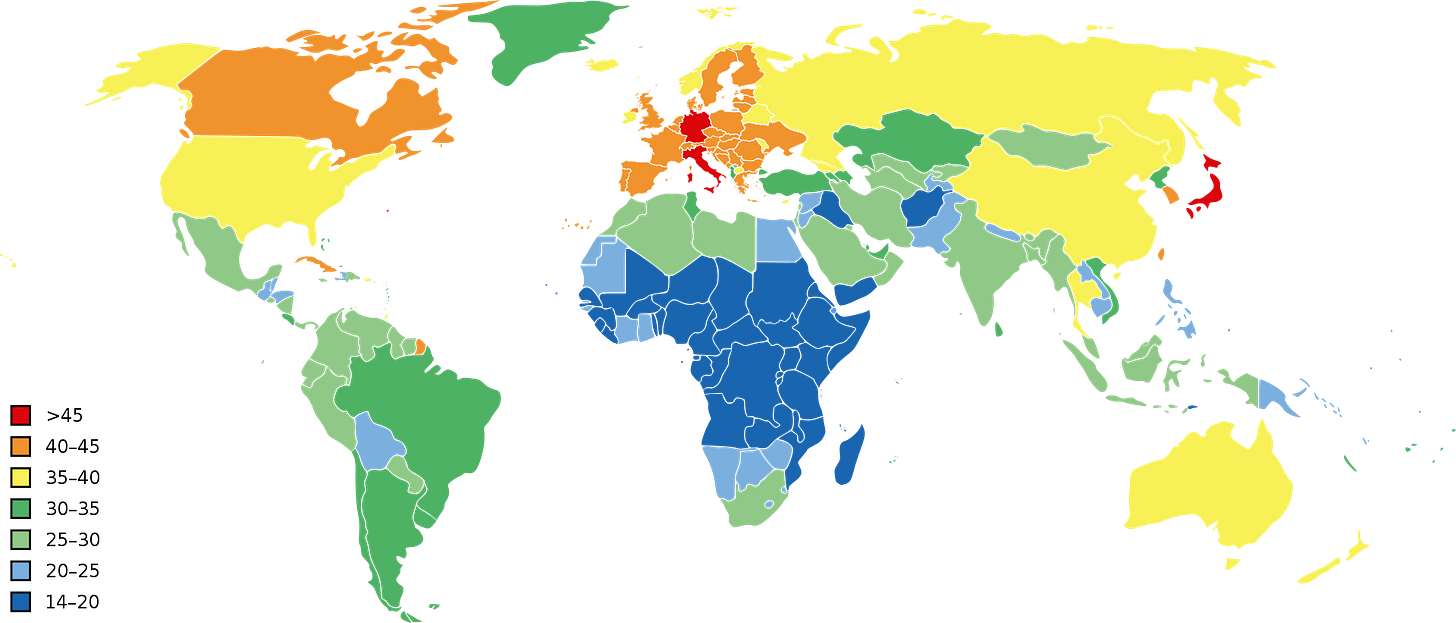
The primary issue comes with the inclusion of another factor, the lengthening of human lifespans, added in. Lifespan has increased over the past 200 years, more than doubling in many places, and in some cases increasing by over a third just since 1950. Thus, these two factors together mean the median age has increased country by country, getting as high as almost 50 years of age in Japan.
Median age by country, CIA World Factbook, 2016 est (taken from wikipedia)
The first concern that comes to many people’s minds given this fact is that there will be more dependents as defined by those past retirement age. Retirement age as a defining life event is such a well-ingrained concept in many people’s minds that efforts to change it are often met with fierce resistance. However, retirement age is in reality a social construct which could be adjusted to prevent economic collapse if people living longer also remained functional for longer, and evidence shows that people may voluntarily work past retirement age if their jobs are well-paid, non-stressful and fulfilling. The real problem is that despite living longer people do not see a later age of onset for most chronic diseases, and thus societies are not able to adapt via social change alone .
What does this imply? The most clear takeaway is that people are living with chronic diseases of aging for longer, as defined by time between disease onset and death (from any cause). There will also therefor be more time for additional chronic aging diseases which arise as comorbidities, with the majority of those over age 80 having 3 or more chronic diseases at once (see below)(note that this is ignoring Quality of Life (QoL) reducing issues such as sarcopenia which are not officially classified as diseases).
Divo et al 2014
Regarding severity over this duration, medications that exist may reduce disease symptoms and progression rates via targeting signaling pathways associated with the disease, such as metformin to lower blood sugar and increase insulin resistance in type-2 diabetes or ACE inhibitors to lower blood pressure in Chronic Kidney Disease (CKD) and Heart Failure (HF). On the other hand, modern medicine has also brought into existence methods of keeping people alive when diseases have reached a stage to severe to have managed previously, and in-patient costs may be among the highest cost-drivers for elderly patients across the majority of age-groups.
The end result of all of this is that the CDC expects that in the US, >90% of all healthcare spending is related to chronic diseases, the majority of which are age-related (cancer included). This trend is also true in other areas outside of the US (1,2,3). This has even led to morbid cost-savings assessments focused around reducing the total need for such care. But there is a straightforward, ethical, zero-compromise approach possible given improved technology - develop improved medicines which prolong the period of disease free lifespan rather than just post-diagnosis lifespan.
Mainstream drugmakers have long worked towards designing treatments for age-related diseases. They are after all the diseases with the largest patient populations in need, and thus also the largest and most dependable markets. What makes researchers and drug developers under the longevity umbrella different on average is not that they care about diseases of aging, but that they hope to reduce the underlying damage associated with these diseases. To aging researchers it is obvious that HF is synonymous with late-stage aging of the heart and CKD of the kidneys (coupled with synergistic aging of other organs such as blood-vessel stiffening which worsens disease in both cases). To prolong disease free lifespan for a given period, you must reduce biological aging to below the threshold that results in diagnose-able disease for that period. You can contribute to this by removing damaged components which contribute to the aged-state of the tissue such as senescent cells or damaging extracellular plaques or protein modifications, directly reprogramming tissue to return to a youthful state such as in epigenetic reprogramming, adding back in healthy cells or tissue such as stem cell therapies or whole organ transplants, and potentially via preventing future forms of aging damage via certain gene therapies and the like. Regardless, let’s consider a thought exercise.
Jane Doe is an average health middle-aged woman in the US. She falls at the 50% mark on the graph regarding co-morbidities above. She will soon, with current technology, get diagnosed with her first chronic disease at age 50, then her second at age 65, third at age 75, and she will die at 80. For this model let’s assume the cost of the three diseases are the same, the cost of 2 diseases is twice that of 1, and also let’s not factor in the increase in cost likely to occur with worsening over time for simplicity sake. Jane will have 30 total life years spent with disease 1 (suppose its Type-2 diabetes), 15 with disease 2 (let’s say CKD), and 5 with disease 3 (perhaps HF), thus 50 total disease-years. Let’s also assume that her ability to work was inhibited 50% by her first disease, though she still worked to some extent until 65. Assuming she began working at age 20, she would have (50-20)+(0.5*(65-50))= 30+7.5= 37.5 productive work years out of an 80 year lifespan. So that’s 50 disease-years in terms of cost to the system, and 37.5 work productivity years in terms of contribution to the system (or just under 50% of years contributing).
Now, new technologies arrive which manage to reduce the total amount of aging damage in tissues sufficiently to increase disease free lifespan by 30 years in each case (and also have arrived for other aging diseases, thus pushing out those which she may have gotten if she had lived longer as well). They repair and rejuvenate underlying tissue, but unfortunately some forms of damage still cannot be targeted so eventually the tissue ages and gets disease. In this case Jane gets T2D at age 80, CKD at 95, HF at 105, and dies the day that she becomes a supercentanarian. She thus still has 50 disease-years, but this time that is smaller relative to her total number of years alive, at 50/110=5/11 vs 50/80=5/8. If she retires at 65 she will have had 45 productivity years, increased slightly from baseline given that she was not held back for the last 15 by having a chronic disease. Given how healthy she is at 65 though, perhaps there is a 50% chance she decides to continue to work until her first chronic disease at age 80, adding another 7.5 probability-adjusted productivity years for a total of 52.5 productivity years in total. This is still just less than 50%. And her total disease free life years is now 80, and at 8/11 of her lifespan is much larger than the previous 5/8.
*One notable problem with the above example is that it assumes timely use of anti-aging damage therapies, likely based on some biomarkers ahead of disease diagnosis. However, if treatments are prescribed in reaction to disease onset and then proceeded to rejuvenate the tissue in a timely manner and temporarily eliminate the disease, the effect would be similar.
In a third, more extreme scenario, Jane lives at a time where known aging diseases are eliminated. Her diseases listed above are treated effectively with techniques which repair and rejuvenate tissue, and in the event that select untreatable forms of damage accumulate excessively a replacement organ can be provided. However, some disease (for the purpose of this discussion) is still not curable, with a median age of onset of 170, and with an average of 30 years between onset and death (the standard deviation is of course likely to be much larger in this case, and many other forms of death have become somewhat more common versus aging diseases, but Jane is exactly average so we will assume the mean for her).
Given that the medical system is so effective at treating most things she could otherwise get she may have less comorbidities over the 30 years, however even if she still had 50 disease years total it would now represent only 1/4 relative to her lifespan (less then half versus when she died at 80). She spends 85% of her life disease free, 170 out of 200 years. and regarding productivity, perhaps retirement age would have gone up given that 65 is now not even middle age, though more likely a combination of reduced demand for manufacturing labor due to due to automation and reduced demand for services sector labor due to fewer dependents overall means the concept of retirement could be traded for majorly reduced hours of work. But, let’s assume the current system remains in place, where Jane works full time from 20 to 65 and then has a 50% of choosing to work at any time post retirement age. This will mean she has (45+((170-65)/2))= 45+52.5= 97.5 productive years, which is actually still slightly higher than in the prior scenarios.
What does this mean at a population level? Assuming a relatively equal number of people of any age (reasonable based on current birth rates in the US) it means that in the last scenario ~85% of people do not have any chronic disease, whereas in the current scenario it’s closer to ~62.5% (80 years - 50 years) (Actual figures show that it is currently even worse than this). Assuming they are all capable of working if they are over 20 years old, that means ~75% are not dependents based on these two factors. That’s versus closer to 50% now (43.75% based on age 1-20 and 65-80 being dependents, though this isn’t including those who need to retire earlier due to disability). Thus, the demographic crisis is reversed, as the % of people who are at a productive biological age has been massively increased.
These assumptions are captured in the tables below.
Table 1: Assumptions and Total Disease/Productivity Years
Table 2: % Lifespan by Disease Years and Productivity Years
This effect is in fact more powerful purely regarding improving the dependency ratio than a baby boom. Assume now that starting today the Total Fertility Rate went up to 5 per woman, and remained that way for 65 years. For simplicity the population I’ll use in the example is 80 million people, 1 million at each age. The post-work population is 15M. At an average age to first child of ~25, there was a 2.5x population growth in the 40-65 cohort and thus we have 25M*2.5=62.5M. The 15-40 cohort is (2.5^2)=6.25x larger, thus the productive group age 20-40 = 20M*6.25=125M people. That gives a total of 187.5M productive working age people versus 15M old-age, way more. But, the 0-15 age group is (2.5^3)= 15.625 larger, or 15M*15.625= 234.375M, + 5*6.25= 31.25 age 15-20, for a total 265.625M dependent minors - significantly more than the total productive working age population. Of course, difficulties in dealing with a large young population are very different than dealing with a large old population. But the reality is that high birth rates have traditionally resulted in high dependency ratios (which are largely shouldered by women). This can also be seen below, observing that the highest dependency ratios correlate with lower median age when compared to the map above.
Dependency Ratio, Our World in Data, https://ourworldindata.org/age-structure
While thousands of years of human history have ingrained a kind of societal credo that procreating more is the only way to improve population decline, I’m confident that the power of the rejuvenation and repair approach will take hold given the severity of the problem. However, it will take the introduction of these types of therapies into the medical mainstream to catalyze the realization by epidemiologists and sociologists that this can happen, and thus is even worth considering. Just one more reason that we are at the time in history where creative people must take risks and initiatives in the aging space.
Note: These models are simplified to represent basic concepts in theoretical population dynamics. However, I’m a founder/biologist, not an demographer, thus I would welcome any suggestions on additional considerations or issues with the current approach.